When it comes to bone health, calcium is usually the first nutrient mentioned. And rightly so: this mineral is an essential component of bone structure (12). However, calcium does not act alone: its assimilation and integration into bone tissue depend, among other things, on several other key nutrients.
And without an efficient digestive system and an intestinal microbiota where there's a balance between good and bad bacteria, the absorption of these nutrients can be compromised. At Clinique Épithélia (link home page), digestive health is considered a fundamental pillar, not only for daily digestive comfort, but also as part of an overall approach to chronic disease prevention... and even to support bone health.
Why worry about bone health?
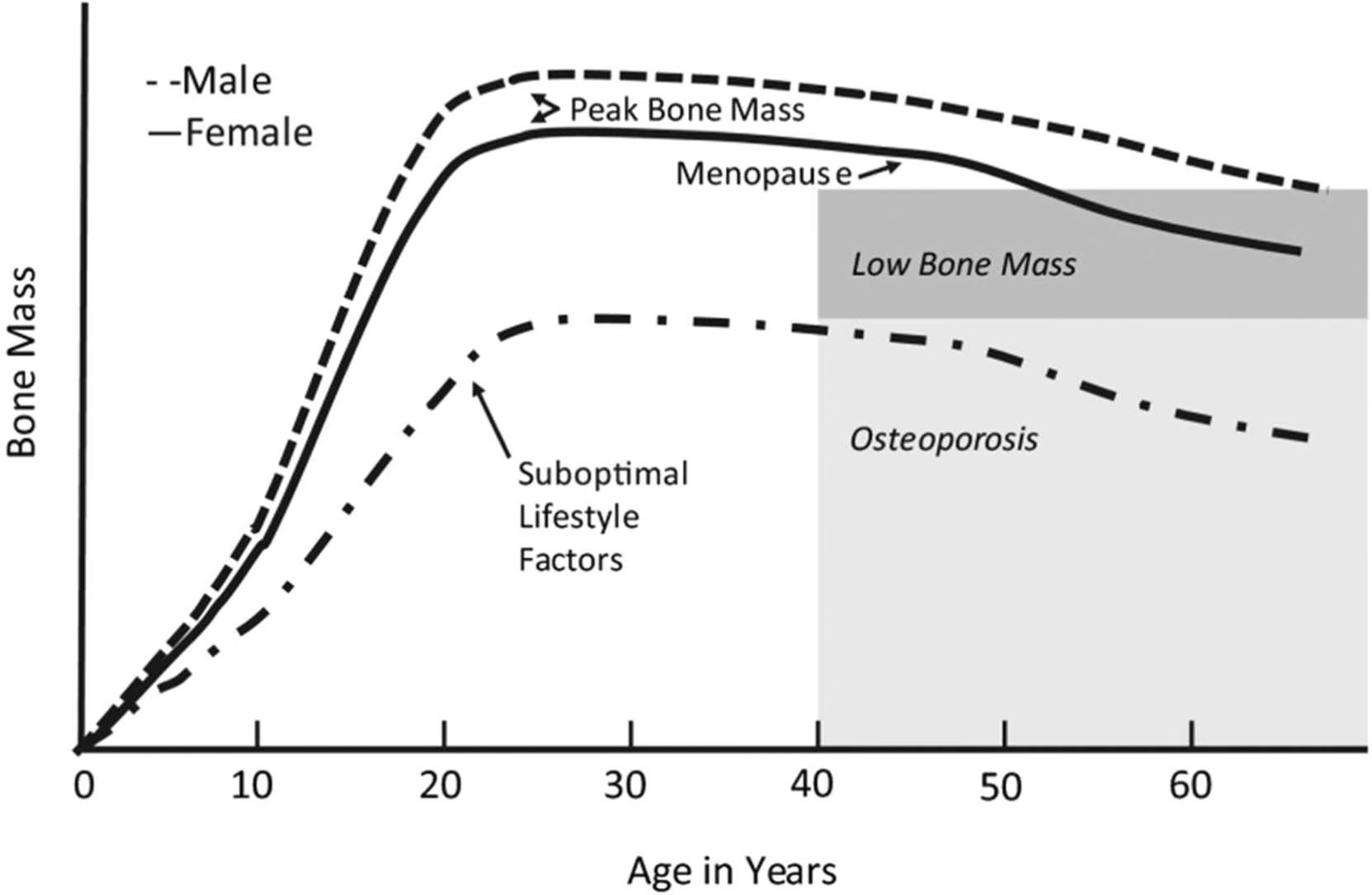
Bones are a living, active structure, constantly reshaped throughout life, and contribute not only to posture and mobility, but also to maintaining vitality in everyday life. Although the risk of osteoporosis is higher in the elderly, prevention begins in childhood. (4) (7)
Into your twenties
Bone density develops (7). This is an important period for maximizing bone density, as it is impossible to increase it afterwards.
Between the ages of 20 and 50
Bone density remains relatively stable, and the priority is to maintain it (3) (7). This period represents a strategic opportunity to support the bone structure and prevent premature bone loss, particularly through lifestyle choices.
After 50 years
Bone mass loss accelerates, particularly in women after the menopause. (7)
Preserving bone health helps maintain strength, mobility and independence over the years. This depends on physical activity, nutrition and... efficient digestion. The aim is therefore to maximize bone mass in the early years, and to slow the loss of bone mass that comes with age. (3) (4) (12)
Vitamins and minerals essential for healthy bones
Calcium never works alone, but rather in synergy with other nutrients. For it to reach its destination - the bones - several other nutrients are essential.
Nutrient
Role
Rich foods
Calcium
The main component of bone structure, it ensures the solidity and rigidity of bones (12).
Dairy products, enriched plant drinks and yogurts, cooked spinach
Vitamin D
Promotes calcium absorption in the intestine. Without it, a significant portion of the calcium consumed is simply evacuated (4) (7) (12)
Cod liver oil, salmon (especially wild), trout, fortified milk or vegetable drink, supplements to consider (to see the recommended daily allowance and what the science says about supplements, see our article “What's new in vitamin D?)
Vitamin K
Directs calcium where it needs to go: into the bones, not the arteries. (1)
Cooked green vegetables (spinach/kale, broccoli, Brussels sprouts, kale, asparagus, okra, green beans), kiwi, parsley
Magnesium
Activates vitamin D in its active form, which is necessary for calcium absorption (9).
Spinach (cooked), hemp and pumpkin seeds, lima and white beans, tuna, quinoa, almonds and cashews, dark chocolate, avocado



How does the microbiota play a role in bone health?
Even when consuming the right nutrients, inefficient digestion can reduce their absorption and compromise their utilization by the body. The intestinal microbiota plays an active role in this process: certain bacteria promote the absorption of calcium, magnesium and vitamins D and K (2).
An imbalance in the microbiota, increased intestinal permeability («leaky gut») (link to leaky gut article), irritable bowel syndrome (IBS) (link to IBS article) or inflammatory bowel disease (IBD), for example, can ultimately affect bone health (8) (11).
Numerous studies underline the central role of the intestine in mineral absorption and overall health, including bone health (5).
Bone health also depends on... muscle mass
Bone strength depends not only on the nutrients listed above and the intestinal microbiota, but also on the maintenance of muscle mass. Bone and muscle work in synergy. (3) As with bone density, muscle mass also tends to decline with age.
From age 30
A gradual decrease is observed from 0.3 to 0.5% per year. (6)
After 50 years
This loss can reach 2 % per year. (10)
Why is it important? Maintaining good muscle mass contributes directly to bone support, good posture, strength, energy and staying active longer without limitations. (3)
How can nutrition support bones and muscles?
Epithelia's dietitian-nutritionists - Digestive Health Clinic recommend several simple gestures:
Opt for a varied diet
Promotes a balanced microbiota and optimizes digestion and absorption of key nutrients. The aim is to find:
- Color! Aim for the 7 colors of the rainbow every day.
- Fiber (fruits, vegetables, whole grains, legumes, nuts and seeds): the preferred food of good bacteria.
- Good fats (avocado, olive oil, fish and seafood): anti-inflammatory allies.
- Fermented foods (kefir, sauerkraut, sourdough bread, yogurt): direct sources of good bacteria.
Eat enough
In the event of an energy deficit, the body limits certain functions, including the maintenance of bone density.
Promote a protein-rich diet
Essential for preserving muscle and bone mass.
Regular physical activity
Exercise stimulates bone renewal and helps preserve muscle mass.
Personalized support
Taking care of your microbiota also means taking care of your overall health, and therefore your bone health. Personalized support enables dietary recommendations to be adapted to specific health conditions and nutritional needs. Consult a team nutritionist-dietitian.
Recipes with foods rich in calcium, vitamin D, vitamin K and magnesium
References
1. Adams, J., & Pepping, J. (2005). Vitamin K in the treatment and prevention of osteoporosis and arterial calcification. American Journal of Health-System Pharmacy, 62(15), 1574-1581. https://doi.org/10.2146/ajhp040357
2. Barone, M., D'Amico, F., Brigidi, P., & Turroni, S. (2022). Gut microbiome-micronutrient interaction: The key to controlling the bioavailability of minerals and vitamins? BioFactors, 48(2), 307-314. https://doi.org/10.1002/biof.1835
3. Carter, M. I., & Hinton, P. S. (2025). Physical Activity and Bone Health. Missouri Medicine, 111(1), 59. https://pmc.ncbi.nlm.nih.gov/articles/PMC6179512/?utm_source=chatgpt.com
4. Cashman, K. D. (2007). Diet, Nutrition, and Bone Health. The Journal of Nutrition, 137(11), 2507S2512S. https://doi.org/10.1093/jn/137.11.2507s
5. Hadadi, N., Berweiler, V., Wang, H., & Trajkovski, M. (2021). Intestinal microbiota as a route for micronutrient bioavailability. Current Opinion in Endocrine and Metabolic Research, 20, 100285. https://doi.org/10.1016/j.coemr.2021.100285
6. Harvard Health Publishing (2016, February 19). Preserve your muscle mass . Harvard Health; Harvard Health. https://www.health.harvard.edu/staying-healthy/preserve-your-muscle-mass
7. Hereford, T., Kellish, A., Samora, J., & L. Reid Nichols (2024). Understanding the Importance of Peak Bone Mass. Journal of the Pediatric Orthopaedic Society of North America, 7, 100031-100031. https://doi.org/10.1016/j.jposna.2024.100031
8. Jha, S. S., Jeyaraman, N., Jeyaraman, M., Ramasubramanian, S., Muthu, S., Santos, G. S., da Fonseca, L. F., & Lana, J. F. (2025). Cross-talks between osteoporosis and gut microbiome. World Journal of Orthopedics, 16(3). https://doi.org/10.5312/wjo.v16.i3.102274
9. Uwitonze, A. M., & Razzaque, M. S. (2018). Role of Magnesium in Vitamin D Activation and Function. The Journal of the American Osteopathic Association, 118(3), 181. https://doi.org/10.7556/jaoa.2018.037
10. Von Haehling, S., Morley, J. E., & Anker, S. D. (2010). An overview of sarcopenia: facts and numbers on prevalence and clinical impact. Journal of Cachexia, Sarcopenia and Muscle, 1(2), 129-133. https://doi.org/10.1007/s13539-010-0014-2
11. Wagatsuma, K., Yamada, S., Ao, M., Matsuura, M., Tsuji, H., Iida, T., Miyamoto, K., Oka, K., Takahashi, M., Tanaka, K., & Nakase, H. (2019). Diversity of Gut Microbiota Affecting Serum Level of Undercarboxylated Osteocalcin in Patients with Crohn's Disease. Nutrients, 11(7). https://doi.org/10.3390/nu11071541
12. Weaver, C. (2016). Nutrition and bone health. Oral Diseases, 23(4), 412-415. https://doi.org/10.1111/odi.12515






